By Maggie Paczkowski, Program Director, Cancer Registries
On World Cancer Day, we are given the opportunity to reflect on the ways society addresses and understands cancer, with the goal of one day eradicating it as a leading cause of death around the globe. One of the most overlooked – yet valuable – aspects of determining cancer incidence and treatment is better cancer data. It’s not as flashy as some of the elements of cancer control, but it is one of the most crucial. Population-based cancer registries (PBCR) provide a clearer picture of the types of cancer, where they are occurring, and amongst which populations they are most prevalent in a given community. The truth is: current, correct and comprehensive data is key to understanding cancer.
There are three primary forms of cancer registries: hospital-based, pathology-based and population-based registries. The data collected through strong partnerships between laboratories and diagnostic centers, public and private hospitals and public health authorities, is the foundation for any cancer registry. And while each registry has its own benefits and drawbacks, population-based registries are the most robust for cancer control and planning.
Hospital-Based Cancer Registries
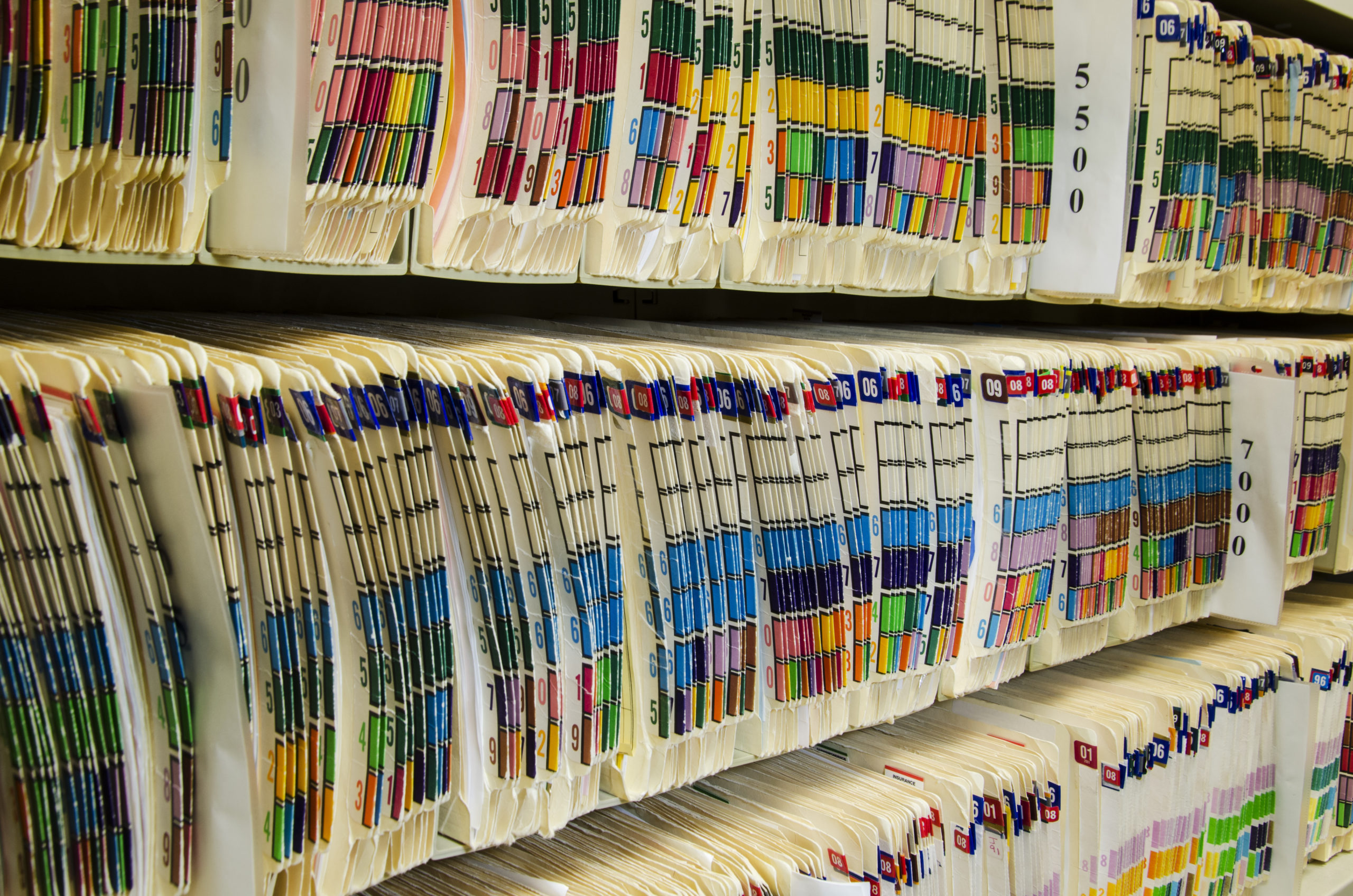
Hospitals and clinics diagnose and treat cancer patients, keeping paper or electronic records of patient information. For example, when a patient with suspected cancer arrives at a hospital or clinic, health care professionals will consult with the patient, ordering any necessary testing or referring the patient to another hospital that can provide diagnostic services if one exists. During this process, information about the patient is collected and put into what is known as a medical record.
Benefits: This information forms the basis for hospital-based cancer registries. Such registries hold critical information on patient burden and allow hospitals to know what medication and how much is needed, what diagnostic equipment is required, as well as the human resources needed to support patient care.
Drawbacks: Often, there are one or two major cancer or specialty hospitals in low- and middle-income countries (LMIC) and the types of cancers these hospitals see are reflective of the patients that travel and seek treatment there; they are likely not reflective of the types of cancers occurring in the population overall and might miss many cancer cases. Put simply: community members without access to hospital care or who seek treatment outside the hospital system, will not be counted in hospital-based registries.
Pathology-based Cancer Registries
When a patient with suspected cancer seeks health care, the health care provider can take a biopsy of the cancer site, if possible and send this sample to a pathology center or laboratory to be assessed for the presence of cancer using a technique known as a histology. The lab then keeps information on each of the samples it has been sent to form the basis of its cancer registry.
Benefits: Pathology-based cancer registries are critical not only for collecting information on diagnosed cancers in a country but also for understanding the diagnostic capacity of countries.
Drawbacks: The information in these registries can be used to give a “snapshot” of the types of cancers occurring in a population but cannot be used to provide us with the estimates we need for planning because they only identify cancers using a specific type of diagnosis. A simple example is a commonly used diagnosis practice: The biopsy. In many cases, sometimes due to the stage of the cancer or a patient’s ability to pay, a biopsy is not taken. In other cases, a biopsy isn’t the best tool for diagnosis, and an MRI might be better. This will inevitably skew the types of patients (those that are wealthier with better access to care) and cancers (cases that are less advanced and easier to diagnose) that will be included in the registry.
Population-Based Cancer Registries
This brings us to PBCRs, which build on the data generated by hospital and pathology-based cancer registries by bringing in more information on the population in which these cancers are occurring. PBCRs are usually located in major cancer hospitals but they can also be located directly within government agencies like ministries of health or universities.
Benefits: No matter where they are housed, one central principle differentiates a PBCR from the other two types of registries: each PBCR tracks all cancers occurring among a population in a geographically pre-defined area, and therefore, can give public health authorities a clearer picture of the cancers occurring.
Within each PBCR are specialized staff—cancer registrars—who have been trained to read medical records and summarize information related to the cause and stage of the cancer. These registrars travel periodically to health centers that diagnose cancer, reviewing medical records and abstracting the needed information. Registrars also periodically follow up with patients to obtain information on treatment and mortality, critical for calculating survival rates. This community-based data can then be validated for quality and used to calculate important information like cancer incidence rates which inform decisions on strategies for clinical management and palliative care for people living with illness.
In addition to working with hospitals and health centers, PBCRs also retrieve mortality information from the country’s civil registration and vital statistics system. This information is not only important to supplement the data collected from hospitals and diagnostic facilities (finding cases they may have missed), but it is important to understanding whether the patients are still alive, allowing the calculation of survival rates. Without survival rates, countries have little information on whether their screening or treatment programs are effective at reducing cancer deaths.
Through the Data for Health Initiative, the Cancer Registries program at Vital Strategies collaborates with countries to strengthen the systems, infrastructure, human resources, and technical expertise necessary to support robust PBCRs. In countries like Myanmar and Tanzania, we are working alongside partners and ministries of health to strengthen data collecting methods and long-term financial and operational planning. Vital Strategies support for population-based cancer registries extends beyond these two countries through the Global Grants Programs. Countries who are not participating in the Data for Health Initiative and are interested in working with our team to strengthen their PBCRs can refer to the GGP website: https://www.d4hglobalgrantsprogram.org/ in spring 2021 to learn about funding opportunities.
To learn more about Vital Strategies’ Data for Health Initiative, please visit vstrategystage.wpengine.com/programs/data-for-health/ and follow us on Twitter @VitalStrat.
The Data for Health Initiative is a global effort supported by Bloomberg Philanthropies and the Australian Department of Foreign Affairs and Trade. It provides technical assistance to low- and middle-income countries worldwide to improve public health data systems at the national level, including improving civil registration and vital statistics systems, maximizing the use of data to enhance public health policymaking and decision-making, establishing and strengthening national cancer registries and more. Vital Strategies serves as an implementing partner.