In 2018, 67,367 people in the United States died as a result of overdose, exceeding all other forms of accidental-injury deaths in the nation. Vital Strategies partners with state and local governments and communities to design and implement tailored, science-backed solutions for achieving significant and sustainable reductions in overdose deaths. Our work includes supporting the adoption and scaling of harm reduction services, as well as a range of medical, legal, and social interventions.
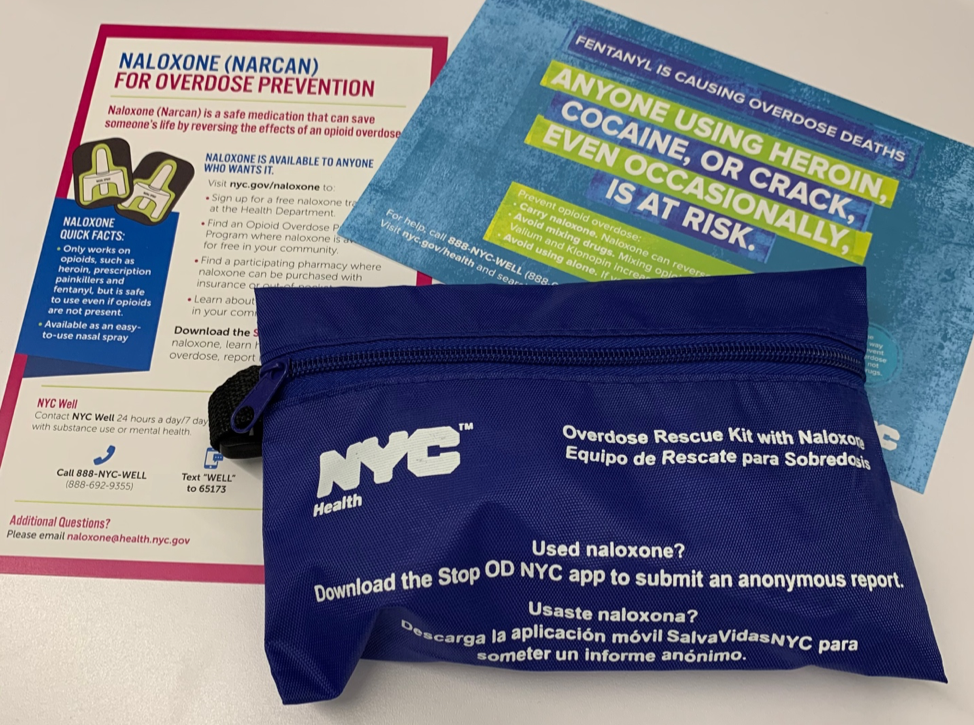
On January 27, Vital Strategies’ Overdose Prevention Program hosted a naloxone training in our New York office to educate staff on the opioid epidemic and what they can do in their communities to prevent fatal overdose and help save lives. We sat down with Esther Mae Rosner, Program Officer of Vital Strategies’ Overdose Prevention Program, to learn more about naloxone and the importance of these trainings.

1. What is naloxone and how does it reverse opioid overdose?
When a person takes an opioid, it binds to specific receptors in the brain. Naloxone is an opioid antagonist which means it binds to the same receptors as the opioids and temporarily blocks their effects.
One of the key features of an overdose is shallow breathing, or a person who has stopped breathing altogether. After naloxone is administered by either nasal spray or injection, a person will usually start breathing regularly within 2-8 minutes.
Naloxone only works if the person is overdosing from an opioid, such as prescription drugs like oxycodone, or street drugs like heroin and fentanyl. Naloxone does not have any other side effects, other than blocking the effects of opioids; it is very safe and has been used for decades in emergency medicine and post-surgical care, but now anyone who has been trained can use it and potentially save a life.
2. Why are Naloxone trainings important for the general public?
Overdose is one of the leading causes of preventable death in the US and data reveals that opioids are involved in at least two-thirds of those deaths. The sheer volume of loved ones who’ve been lost is devastating, but what’s also tragic is that these lives could have been saved because there is this medication that can reverse an opioid overdose and save lives. Naloxone trainings are important for the general public because the more widely distributed this medication is, the fewer fatal opioid overdoses will occur; we know people will use it and save lives.
Public naloxone trainings are also an important beginning for conversations about drug use. Drug use has been so stigmatized in the US that people are often too ashamed to ask questions about how to stay safe and how to ask for help when they need it. I conducted naloxone trainings for nearly 9 years, first on outreach as a volunteer at syringe service programs, then as a counselor in substance use treatment, and then as a social worker at a harm reduction program. At many trainings I had countless people attend simply to learn about overdose and drug use
3. What other topics are usually covered at a community naloxone training?
Community naloxone trainings open a space for people to ask questions and learn about issues that are too often swept under the rug, like the intersection of drug use and race. This is a frequent conversation during trainings I provided in New York City. In the US, the war on drugs disproportionately impacts people of color, evident by the fact that fatal overdoses are concentrated in communities that are low-income and communities of color. This stands in stark contrast to the story we often see portrayed in the media that paints the overdose crisis as a tragedy that only hurts white suburban and rural communities.
Naloxone trainings are not simply a vehicle for showing people in a few minutes how to administer this life-saving medication — these trainings address the broader overdose landscape happening in communities and catalyze conversations about who this crisis is impacting, about who has access to resources like naloxone and medication treatment, and why.
4. Can these trainings be conducted across the United States?
This question highlights a very important problem – the laws that govern naloxone distribution vary widely from state to state, despite its status as a safe and easy to use medication. While most states have adopted some kind of naloxone access law in recent years, there are some settings where only prescribers or pharmacists are authorized to dispense or distribute naloxone for third party administration. Many states have also enacted protections for people who distribute or administer naloxone in the community, but these protections are not universal. This can be a barrier for community organizations that work directly with people who use drugs to promoting naloxone access. Moreover, many states do not adequately fund naloxone distribution and education, placing the burden on providers and community organizations.
In states facing legal and financial barriers to community-based naloxone distribution, efforts need to be more targeted and strategic to ensure naloxone reaches those who need it most, and especially including people who use drugs and their loved ones.
5. How is Vital Strategies working to expand Naloxone access and education?
The Overdose Prevention Program at Vital Strategies views expanded naloxone access across sectors and into communities as an essential intervention for reducing overdose deaths. We are working with state and local governments to reduce barriers to naloxone access with an emphasis on getting the medication into the hands of people who use drugs and those closest to them.
On the ground, this means providing naloxone training and distribution to those who are most vulnerable to overdose, including people who have recently experienced a period of abstinence and as a consequence, their tolerance to opioids has been reduced, whether they have been released from detention settings, or leaving a substance use treatment program. We are also working with emergency departments to get naloxone to people who have come to the hospital following an overdose, and with community organizations that work with people who use drugs.
6. What are other ways people can work in their communities to prevent overdose?
Start conversations about overdose with people in your community. Find out where overdoses are happening and to whom they’re happening. Ask questions about what resources are available, if they’re not available, ask why. Listen to the voices of people who use drugs they are on the front lines of the overdose crisis.
Be mindful that these conversations will not be light. Overdose comes at a high cost to the people living closest to it. These conversations will require your compassion. Remind your community that people who use drugs are not people to cast aside under the label of addicts or drug users – these are our friends, our families, our neighbors, and our coworkers. People who use drugs are part of our communities. Preventing the loss of another person to a fatal overdose is worth the time it takes to have this conversation. Let’s talk.
To learn more about our Overdose Prevention Program visit: https://www.vitalstrategies.org/programs/overdose-prevention/